- coronavirus
- Posted
Evidence of COVID-19 infections in poorly ventilated spaces
The airborne transmission of COVID-19 may be a risk in enclosed spaces with air recirculation or poor fresh air ventilation, with one study concluding that airborne transmission may have occurred in 48.3% of people in a poorly ventilated office and 34.3% of passengers on an air conditioned bus.
This report is a more detailed version of an article by Jeff Colley published in the Sunday Times on 3 May.
A team of Chinese and US academics investigated COVID-19 transmission rates from two early COVID-19 outbreak events in Zhejiang, a Chinese province three hundred kilometres east of Hubei.
The first event was a 100 minute round trip on 19 January to and from an outdoor worship event in Ningbo City. The 293 attendees at the event, which was moderated by five monks, included 126 who travelled by bus, on a pair of buses with air conditioning systems operating in re-circulation mode. Fifty-nine passengers travelled on bus one and 67 on bus two, with the remaining 167 travelling by other means. The only attendee who had been exposed to people from Wuhan before the event was the source patient, a 64 year old woman who sat on bus two, and who became the first event attendee to become symptomatic, on the evening after the event.
The study, which was released as a preprint before formal peer review had been conducted, identified seats for all 67 passengers on bus two, each of whom took the same seats for the return journey. Twenty-three passengers tested positive for coronavirus after the event, including the source patient. None of the 59 passengers on bus one – which served as a useful control group for the study – tested positive. Seven of the remaining 172 attendees tested positive, all of whom were in close contact with the source patient at the event.
There was no statistically significant increase in infections of passengers who had been sitting closer to the source patient, indicating infection may have occurred via re-circulation of air. The passenger sat in the window seat next to the source patient was the only one of 13 passengers sitting in window seats on the passenger’s side of the bus to be infected, while only one of ten passengers sitting by openable windows was infected.
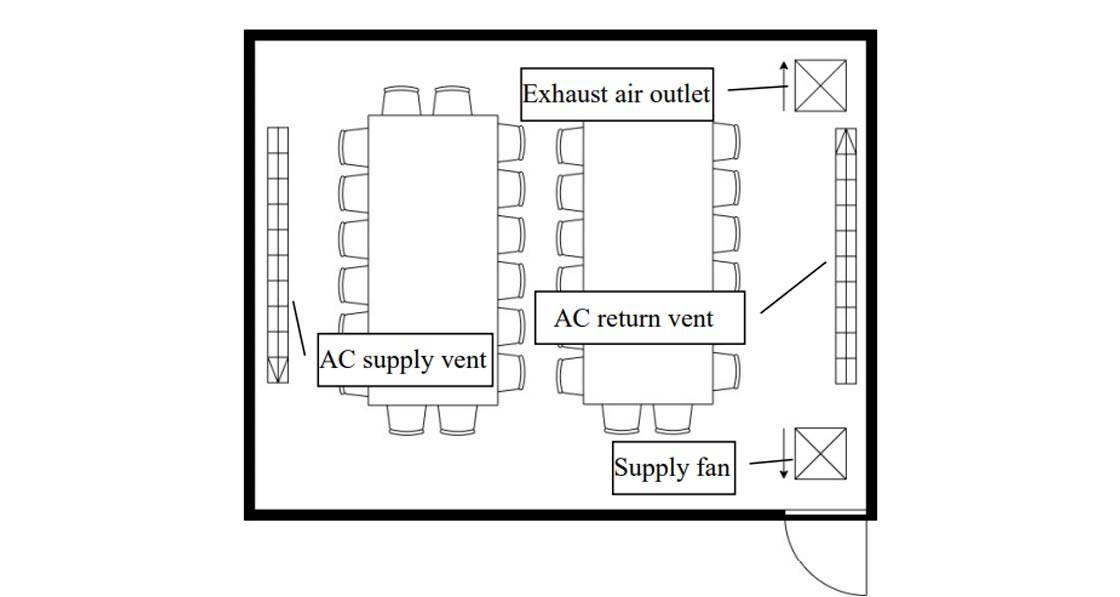
The second event included 30 attendees at a three day workshop in Hangzhou city from 12-14 January, including one trainee who had travelled from Wuhan: a 45 year old woman who was asymptomatic during the event but developed systems on 17 January. The first day of the event took place in a 49 square metre conference room, with the second day in a 75 square metre conference room. Both rooms had air conditioning systems recirculating air during the event, with fresh air introduced for 10 minutes every four hours, which was estimated to lead to a quarter of the air in the room changing.
Trainees reported poor air quality in the conference rooms. The study had limitations, such as a lack of information on seating arrangement, which meant that infection by close contact couldn’t be ruled out, but the authors concluded that airborne infection was highly likely, given the dramatic infection rate. “The particularly high attack rate, approaching 50%, is alarming and suggests large community gatherings, especially those in enclosed settings with minimal air ventilation, should be limited,” the report stated.
The findings are echoed in another preprint of a study on an early COVID-19 outbreak at a restaurant in the southern Chinese city of Guangzhou on Chinese New Year’s eve, 24 January. The study involved a lunch service for a family who had travelled from Wuhan, with five people from two families sat at adjacent tables becoming infected. The study included analysis of CCTV footage of the occasion, a seating plan, and detailed analysis of air movement in the restaurant, which included an air conditioning system recirculating air with no fresh air ventilation. The CCTV footage found no evidence of close contact or fomite (surface) spread during the lunch. “The infection distribution is consistent with a spread pattern representative of exhaled virus-laden aerosols,” the study concluded. “Aerosol transmission of SARS-CoV-2 due to poor ventilation may explain the community spread of COVID-19.”
According to the HSE, the evidence does not currently indicate airborne transmission of COVID-19. “According to current evidence, COVID-19 virus is primarily transmitted between people through respiratory droplets and contact routes,” a HSE spokesperson said. “The WHO has highlighted an analysis of 75,465 COVID-19 cases in China: airborne transmission was not reported.” The executive conceded that airborne spread may however be an issue in specific health care treatments where a patient may generate aerosols. “The virus that causes COVID-19 is spread mainly by contact and droplet. Airborne transmission of the COVID-19 virus is a concern when certain procedures for example placement of an ET tube are being performed. This risk is managed by wearing specific PPE when performing these procedures and by performing them in rooms with controlled ventilation when possible.”
According to Prof Linsey Marr, an aerosol scientist at Virginia Tech, the evidence for airborne transmission of COVID-19 beyond such specific healthcare settings should not be ignored. “I don't think we can rule out airborne transmission of COVID-19, especially in close contact situations and in spaces with poor ventilation for the number of people present. In fact, there is mounting evidence that airborne transmission is occurring. There isn't actually any direct proof of transmission by large droplets either.”
Meanwhile, REHVA, the Federation of European Heating, Ventilation and Air Conditioning Associations, has published guidance on how to operate and use building services in order to prevent the spread of the coronavirus in workplaces, including advice to increase mechanical ventilation rates in general and in toilets in particular, turn off recirculation on air conditioning systems, and to open windows much more than normal, in particular in buildings with no mechanical ventilation.
Leading building services engineer Declan Alcock of Varmings said that while remote working may reduce the risk of airborne spread in offices due to lower occupancy levels, short term guidance focused on increasing ventilation rates and avoiding recirculation of air. “Depending on how long COVID-19 is with us there may be long term considerations, such as a rethink on the design of HVAC systems for new buildings and retrofitting of systems in existing buildings.”






